以铜为鉴,可以正衣冠;以人为鉴,可以明得失;以史为鉴,可以知兴替。
byWilliamH Donovan, MDAbstract
Summary:
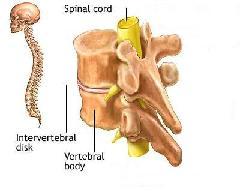
This special report traces the path of spinal cordinjury (SCI) from ancient times through the present and provides anoptimistic overview of promising clinical trials and avenues ofbasic research. The spinal cord injuries of Lord Admiral SirHoratio Nelson, President James A. Garfield, and General GeorgePatton provide an interesting perspective on the evolution of thestandard of care for SCI. The author details the contributions of awide spectrum of professionals in the United States, Europe, andAustralia, as well as the roles of various government andprofessional organizations, legislation, and overall advances insurgery, anesthesia, trauma care, imaging, pharmacology, andinfection control, in the advancement of care for the individualwith SCI.
Keywords:Spinal cord injuries, Spinal cord medicine,History, Munro, Donald, Guttman, Ludwig, Young, John, Bors, Ernest,Comarr, A. Estin, Rossier, AlainGo to:INTRODUCTION
As with most other topics, in order to acquire acomplete understanding of spinal cord injury (SCI), one mustappreciate the events that comprise its past, present, and future.This “trinity of time” for SCI has a most interesting past, anexciting present, and a very promising future.
Go to:THE PAST—AN AILMENT NOT TO BE TREATED
Nowadays, in science as in industry, much emphasis isplaced on the future and the shaping of the present so that itleads directly to some desired outcome. Often overlooked in theplanning of such quests are the events that have preceded them andhow they have shaped the present. Understanding those events cangive one a better grasp of the reasons that justify one's pursuits.We tend to forget the admonition of the well-known Spanishphilosopher, George Santayana (1863–1952) who while teaching atHarvard University in the US said, “Progress, far from consistingin change, depends on retentiveness…. Those who cannot remember thepast are condemned to repeat it.” (1)This advice is especially worth remembering when it comes to SCI,which actually has a rich, absorbing past that harks back a longway to roughly 2,500 years BCE. We know this from the writingsinscribed in the Edwin Smith surgical papyrus.
Little if any time is given to this important treatiseduring any of the levels of medical education, ie, medical schoolthrough residency and graduate medical education. Yet, as TrevorHughes explains in his analysis of this document, it is (a) thefirst known record extant that can be called a scientific document,(b) the first known important medical treatise, (c) the firstmedical document concerned with trauma, and (d) the firstdocumentation of cases of spinal cord injury (2).
The scroll was purchased by an American Egyptologist,Edwin Smith, in Luxor, Egypt, in 1862 and then translated from thehieratic by James Henry Breasted (Figure 1), at thebehest of the New York Historical Society and published in 1930(3). The document contains descriptionsof 48 traumatic cases, 6 involving the cervical spine, and 2 ofthose 6 are clearly injuries to the spinal cord. The author has anobvious knowledge of anatomy and experience in the surgicaltreatment of his day. Some have posited the author was Imhotep. Thescribe who copied the original document some 1,000 years later (thecopy Smith purchased) was also knowledgeable and added comments ofhis own. The author explains to the reader (his students) how eachof the 48 cases should be treated, eg, “packing the wounds withfresh meat.” Of special interest to us are his instructions thatthose 2 cases of SCI are not to be treated at all—“an ailment notto be treated” (2).
Figure 1Under the sponsorship of the New York HistoricalSociety, James Henry Breasted translated the Edwin Smith surgicalpapyrus from the hieratic. The translation was published in 1930.Photo is from the Encyclopedia Britannica online at http://www.britannica.com ...In fairness to the author and his therapeutic nihilismtoward SCI, more than 4,000 years ago he was probably dealing withinjuries sustained during battlefield conditions where principlesof triage prevailed and where limited resources were reserved forthose who could be healed and returned to duty. Yet, one cannothelp but be saddened that the author's advice not to treat wasfollowed wittingly or unwittingly down through the millennia thatensued, up until the early part of the 20th century. Examples ofthis nihilistic philosophy can be cited from the records of peoplefamiliar to us in the 19th and 20th centuries. Let us examine 3such well known cases and how they were managed:
1. Lord Admiral Sir Horatio Nelson (1758–1805). Thereis perhaps no British naval hero more revered by Great Britain thanLord Nelson (Figure 2). Havinglost an eye and an arm in the service of his country during thecourse of his numerous naval victories, he finally lost his life,victorious at the battle of Trafalgar, on October 20, 1805. Ondeck, urging on his men, boarding the Spanish man-o'-war that camealongside his flagship, HMS Victory, he was felled by asniper's bullet that entered his chest and spinal cord. He wasimmediately taken below, and the ship's surgeon was summoned. LordNelson told the surgeon, Mr Beatty (in the British Commonwealth,surgeons are addressed as “Mr”), “All power of motion and feelingbelow my chest are gone.” Mr Beatty duly examined his patient,confirmed his SCI and then, no doubt with head bowed, said “MyLord, unhappily for our country, nothing can be done for you.” Onecan safely say that if anything could have been done, it surelywould have been for Lord Nelson. But Mr Beatty was right. Hispatient had “an ailment not to be treated” (4).
Figure 2One example of the therapeutic nihilism towardspinal cord injury care before 1950 is the case of Lord Nelson. Atthe battle of Trafalgar, October 20, 1805, Lord Nelson was felledby a sniper's bullet that entered his chest and spinal cord.Nothing could ...Nelson's victory that day destroyed both the Frenchand Spanish armadas and while it did not stop his nemesis,Napoleon, from his victorious march across Europe, it did ensurethat Nelson's island country would remain safe from any subsequentattack from the sea by L'Empereur. For this, he is recognized by amonument at Trafalgar Square in London, which dominates itssurroundings (5).
2. James A. Garfield (1831–1881), 20th President ofthe United States. Shortly after taking office, Garfield was shotby a disgruntled, passed-over office seeker. The bullet lodged inthe conus medullaris, resulting in paralysis of his legs, bowel,and bladder. Complications ensued and after surviving 80 days, hesuccumbed (6). Despite the medical treatments thatcould be brought to bear at that time, President Garfield'sphysicians, whom some say were more harmful than helpful,accomplished no more than what Mr Beatty was able to do. The 20thPresident had “an ailment not to be treated.” The Museum of theArmed Forces Institute of Pathology has on display a specimen ofthe former President's shattered vertebra (Figure 3). (It alsohas a specimen of the upper cervical vertebrae of John WilkesBooth, murderer of President Abraham Lincoln, who was shot in theneck when captured) (4).
Figure 3(A) Illustration of James A. Garfield, 20thPresident of the United States, who was shot in the conusmedullaris and survived 80 days (6). (B) The museum of the Armed ForcesInstitute of Pathology has on display a specimen of the formerpresident's shattered ...By the time the US entered World War I (April 1917),many combat SCIs had been incurred by the soldiers of the warringparties, and this continued until the armistice (November 11,1918). The famous American neurosurgeon, Harvey Cushing (1869–1939)(Figure 4), writingfrom the 14th General Base Hospital in France, reported that “theconditions were such [that] 80% died in the first few weeks [and]….only those cases survived in which the spinal lesion was a partialone.” The rest had ailments that were not to be (could not be)treated. Cushing and others lamented the defeatist attitude thatprevailed at that time toward SCI among all the health careprofessions (4,7).
Figure 4Harvey Cushing, famous American neurosurgeon,wrote, “The conditions were such that 80% died in the first weeks[and]… only those cases survived in which the spinal lesion was apartial one.” Photo courtesy ...3. General George Patton (1885–1945), commander ofthe US Seventh and then the Third Army during World War II(Figure 5). Avolatile yet eminently successful leader throughout the campaignsin North Africa and Europe, he was involved in a motor vehiclecrash only months after the conclusion of war in the Europeantheater. He sustained a cervical spinal cord injury, possiblyincomplete. Patton knew there was no cure for SCI (an ailment notto be treated). He thus refused all treatment and was reported tohave died from a cardiovascular complication while stillhospitalized (8).
Figure 5General George Patton(1885–1945), Commander of the US Seventh and then the Third Armyduring World War II. He sustained a cervical spinal cord injury ina motor vehicle crash.Finally, as another example of conditions thatprevailed for persons with SCI, even as recently as 1944, there isa poignant memo quoted by Silver: “In the spring of 1944, I wascalled to group headquarters for an interview with the groupofficer, a surgeon of formidable character. ‘Allen,’ he said to me,‘I am sorry to have to inflict this on you, but we have beenordered to open a spinal unit at Leatherhead Hospital and I wantyou to take charge of it. Of course, as you know, they are hopelesscases—most of them die, but you must do your best for them.’ Withthese words of ‘encouragement,’ I returned home sadly”(7).
Although a “cure” for SCI has yet to be discovered,it would be wrong to say that no interest in the pursuit of thisobjective existed prior to the latter part of the 20th century. Aswe will see, that is when the quest for a cure began to be takenseriously by more and more investigators.
Given their historical role of first responders totrauma, it is not surprising that the first group to expressinterest in finding some way of ameliorating the effects of SCI wassurgeons. It is equally not surprising that their proposedinterventions involved surgery. And this mind-set has prevailedeven to the present. During the early 19th century, a controversyarose between two British surgeons, Sir Astley Cooper and SirCharles Bell (Figure 6). Theformer favored operating on the injured spinal cord, arguing thatsince death was inevitable anyway without surgery, nothing was tobe lost. The latter posited that surgery only increased the risk ofdeath and could further damage nerve fibers with any potential toimprove (9).
Figure 6Left: Sir Astley Cooper favored operating on theinjured spinal cord, arguing that since death was inevitable anywaywithout surgery, nothing was to be lost. Right: Sir Charles Bellposited that surgery only increased the risk of death and couldfurther ...Over the next 100-plus years, the topic of reversingthe effects of SCI, when it did appear in the medical literature,was largely centered on the feasibility of operating. Thisprevailed until the last decade of the 20th century, whenpharmacologic treatments made their appearance (10,11). In point of fact, the only reasonthat the issue of surgery dominated the pursuit of finding a curefor SCI over the years was because of landmark discoveries in otherbranches of medicine that continued to make surgery on the injuredspine (or any part of the body, for that matter), as well astreatment of complications, safer and easier. These breakthroughswere numerous, and a thorough discussion is beyond the scope ofthis article; however, it is important to remember that theproblems that they solved were as much of a challenge to theirdiscoverers in their era as the quest for a cure for SCI is to ustoday. I will therefore simply list some of them and commentbriefly.
In the field of microbiology, Louis Pasteur(1832–1895) advanced our knowledge of sterilization as well as the“germ theory” in general (12); Ignaz Semmelweis (1818–1865)demonstrated to skeptics that hand washing and clean techniquecould drastically reduce the transmission of disease, and yet hewas ridiculed in 1849, even by the most renowned pathologist of hisday, Rudolf Virchow (1821–1902), for proposing that invisibleorganisms could cause illness (13); Joseph Lister (1827–1912) appliedthe concept of antisepsis to surgery and wound treatment(14); Robert Koch (1843–1910) provedbeyond a doubt that microbes cause disease (15); William Stewart Halstead(1852–1922) introduced the surgical glove (16); and Alexander Fleming (1881–1955)discovered penicillin and inaugurated the antibiotic era(17).
Although the contributions of Semmelweis, Lister, andHalstead were breakthroughs for infection prevention, clearlyFleming's discovery and the production of the antibiotics thatfollowed had the greatest impact on survival after SCI. Now,infections that became established during the acute and chronicphases of SCI could be eliminated. Conditions prior to theantibiotic era were described by the medical superintendent at theRoyal Star and Garter Home (the first spinal unit in the UnitedKingdom) in 1934: “Any local infection is liable to be followed bya general infection, cystitis, or pyelitis; and pyelitis is almostalways the ‘end condition’ of the paraplegic” (18).
In the field of anesthesia, Sir Humphrey Davy(1778–1829) demonstrated the use of nitrous oxide, William T. G.Morton (1819–1868) the use of ether, and John Snow (1813–1858), theuse of chloroform (19). When the senior surgeon at TheMassachusetts General Hospital, John Collins Warren (1778–1856),allowed Morton to demonstrate “etherization” on his patient whothen felt no pain during the resection of a vascular tumor on theskin over the mandible, he proclaimed with amazement to hiscolleagues “Gentlemen, this is no humbug” (Figure 7a andand7b).7b).The era of painless surgery had begun (13,20).
Figure 7aSenior Surgeon at MassachusettsGeneral Hospital John Collins Warren (1778–1856) allowed William T.G. Morton to demonstrate “etherization” on hispatient.Figure 7bScene believed to be a re-enactment of thedemonstration of ether anesthesia by W. T. G. Morton on October 16,1846. Mr. Holman with surgeons: John Mason Warren, George Hayward,Solomon D. Town-send, John Collins Warren and James Johnson aroundman on ...In the field of hematology, Karl Landsteiner(1868–1943) discovered the ABO blood typing system and later he andAlexander Weiner (1907–1976) discovered the Rh system. Through thedetection of incompatibilities between patient and blood donor, andthereby the avoidance of hemolytic reactions, surgery was madesafer, as were transfusions for any other reason (21).
In the field of imaging, the discovery by WilliamConrad Roentgen (1845–1923) of the x-ray (22), the application of radiography tomyelography by J. A. Sicard (1872–1929) (23), the development of computerizedtomography (CT) scanning by William Oldendorf (1925–1992)(24,25), and the development of magneticresonance imaging (MRI) by Raymond Damadian, A. Reid, and others,all made spinal surgery safer by allowing the surgeon to have moreknowledge of the pathology and more preparation prior to operating(26).
Early treatment for spinal injuries included closedand open methods. Spinal traction was described both in the EdwinSmith papyrus and later by Hippocrates (470–410 BC)(27). In modern times, Sir GeoffreyJefferson (1886–1961) utilized halter traction, while Sir ReginaldWatson-Jones (1902–1972) placed the patient in the prone positionbetween 2 tables (28). W. Gayle Crutchfield (1900–1972)first described skeletal traction in 1933 (29,30). In 1955, Vernon Nickel(1918–1993) and colleagues applied the principle of skeletaltraction, called halo traction, by using the halo vest(31). These methods provided a way ofobtaining closed reduction and of maintaining better alignment ofthe spine, whether the patient was treated operatively or not.
Finally, the techniques of surgery itself improved,providing better reduction of deformity and stabilization over thelast 50 years. If we were to focus on major contributors, one wouldhave to begin with Paul Harrington (1911–1980) (Figure 8) for hisintroduction of a system of distraction and compression rods andhooks. His system was intended for the treatment of scoliosis(32), but spinal surgeons were quick torecognize its capacity to adapt to the treatment of spinalfractures and dislocations, particularly of the thoracolum-barspine (33). Many instruments have beendeveloped in the years that followed, most notably those of RaymondRoy-Camille (pedicle screws), K. Kaneda and K. Zielke (anteriorplates and screws), and Y. Cotrel and J. Dubousset (pedicle screwsand plates) (34,35). That said, however, and despitethe advances in surgical instruments and techniques, the argumentthat began with Cooper and Bell is not completely resolved becausepatients managed without surgery can also have favorable outcomes(36–39).
Figure 8Paul Harrington (1911–1980)introduced a system of distraction and compression rods andhooks.Clearly, it took the accomplishments of many peoplefrom diverse fields to bring us to the point where people with SCIcould be kept alive and treated operatively or nonoperatively withthe prospect of living past the period of the acute injury with analigned and stable spine. At least, the injury to the spinal columncould be treated. The injury to the spinal cord itself, as well asthe organ systems to which it brings innervations, have continuedto pose great challenges.
Some challenges to the latter have been met. Those ofthe former continue to elude us. Nevertheless, as we shall see,progress in the form of treatment of the effects of SCI on thehuman body has been made by many who have given their careers toSCI. I think at least 6 people deserve special recognition fortheir contributions. I call them “heroes of the 20th century.”
Donald Munro (1898–1978) (Figure 9) has beencalled by some the “father of paraplegia” (40,41). Although mortality from SCI wasstill virtually certain (except for very incomplete injuries),Munro was unique among physicians in his day given his interest andcompassion for patients with SCI and his refusal to accept thedefeatist attitude toward them so widely prevalent and articulatedby Cushing. He established the first spinal cord unit in the US atthe Boston City Hospital in 1936 (40). He soon realized that he had tobe more than just a neurosurgeon to his patients. He had to acceptresponsibility to provide for the whole person, who had problemsinvolving multiple organ systems, eg, neurological, urological,orthopedic, psychological, and social. In addition, he had tocoordinate all the rehabilitation efforts to improve self-care,mobility, and reassimilation into society, including educationaland vocational pursuits. Although his vision was not appreciated bymost of the other specialists of his day, he was successful ininfluencing the US army to establish SCI centers at a few hospitals(initially at Oxford-Wingate in Massachusetts), where his methodswere implemented, eg, the use of “tidal drainage” to preventrecurrent urinary tract infection (UTI) (40,41). His success in the treatment of“an ailment not to be treated” served as a model for others whofollowed.
Figure 9Left. Donald Munro (1898–1978) has been calledthe “father of paraplegia.” Photo courtesy of the Society ofNeurological Surgeons. Right. Sir Ludwig Guttmann (1899–1980) wasput in charge of an SCI unit at Stoke-Mandeville...Sir Ludwig Guttmann (1899–1980) (Figure 9) is themost internationally recognized hero of this group. Born inSilesia, a long-troubled part of the globe contested for possessionby Germany and Poland, he trained in Breslau (now Wroclaw) as aneurosurgeon under Otfrid Foerster (1873–1941). His practice andreputation were curtailed by the Nazis. Since he was only allowedto treat other Jews, he became chief of neurosurgery at The BreslauJewish Hospital. He escaped from Germany to England in 1939, and in1944 he was placed in charge of an SCI unit at Stoke-MandevilleHospital. The care of patients with “ailments not to be treated”was never his aim in life, but fortunately, Sir Ludwig was a manwho never backed away from a challenge. In learning as much as hecould about SCI, he drew from the work of Munro and like thelatter, he soon realized doctors treating this illness had to berehabilitationists with a commitment to all the needs of thepatient, not just those within the ambit of one's specialty(42).
Like Munro's, his SCI unit became a model for futurecenters. Great Britain and the rest of the British Commonwealth,Europe, and Asia all modeled their centers after Stoke-Mandeville.Unlike Munro, he strongly believed in proselytizing his experiencesand traveled widely throughout the globe. A great believer inwheelchair sports, he is remembered for founding the Paralympics(42,43).
Australia was one of the places in the BritishCommonwealth visited by Guttmann and it was here that he met alike-minded individual who never refused a challenge and waswilling to commit to SCI, namely Sir George Bedbrook (1921–1991)(Figure 10). LikeMunro and Guttmann, Bedbrook soon realized he had to be arehabilitationist, not just an orthopedic surgeon. He accepted thetask of forming a spinal unit in Perth, Western Australia, andafter a specially designed unit was completed in 1954, he attractedmany talented people who focused their energies on studying andtreating SCI, including John Pearman, microbiologist, and ByronKakulas, neuropathologist (44).
Figure 10Sir George Bedbrook (1921–1991) (standing) wasan orthopedic surgeon who formed a spinal unit in Perth, WesternAustralia. He is pictured here with Sir Ludwig Guttmann (seated).Bedbrook was a dynamic visionary who traveled widely andinfluenced ...Like Guttmann, he traveled widely, supporting theefforts of physicians starting units in Australia, New Zealand, andAfrica and throughout Asia. The efforts of this dynamic visionaryinfluenced the physicians, therapists, nurses, and all whoencountered SCI patients in those parts of the world. I considermyself very fortunate to have worked with him for more than 2 years(9).
Ernest H. J. Bors (1900–1990) and A. Estin Comarr(1915–1996) (Figure 11) areusually considered together because of their numerous contributionsto the field of SCI and their tireless work to providecomprehensive care at both the Long Beach, California VeteransAdministration (VA) Hospital and Rancho Los Amigos Hospital inDowney, California. Their numerous articles on the neurology,especially the neurourology, of SCI remain classic. Bors was bornand trained as a urologist in Prague. Like Guttmann, he was aJewish refugee. He came to the United States and joined the ArmyMedical Corps. Also, like Guttmann, he established comprehensivecare for a large number of patients (45,46). Comarr founded the AmericanParaplegia Society (APS) in 1954 (41).
Figure 11Ernest H. J. Bors (1900–1990)(left) and A. Estin Comarr (1915–1996) (right) both establishedcomprehensive care for a large number of patients with SCI.Courtesy of the American Paraplegia Society.Despite the efforts of Munro, Bors, and Comarr,approaches to treatment of SCI, with some exceptions, remainedfragmented, and comprehensive rehabilitation for SCI failed tobecome widely adopted in the Western Hemisphere until John Young(1919–1990) (Figure 12) resolvedto correct this. Young was greatly influenced by the work ofGuttmann and the directors of European SCI units and was an activemember in what was then the International Medical Society ofParaplegia (now the International Spinal Cord Society), which wasfounded by Guttmann in 1961. With the assistance of J. Paul Thomas,then director of the Medical Sciences Program at the NationalInstitute on Disability and Rehabilitation Research (NIDRR) (Figure13), he obtained a federal grant in 1971 to demonstrate thesuperiority of comprehensive over fragmented SCI care in Phoenix,Arizona. He called this demonstration a “Model System.” Hisaccomplishments were quickly recognized, and more locations weresoon designated by the NIDRR as Model Systems. These Model Systemshave remained in existence over the decades; they now number 14across the US and contain the largest known database on SCI, theNational Spinal Cord Injury Statistical Center database (NSCISC)(47).
Figure 12John Young (1919–1990) (left), with theassistance of J. Paul Thomas (not shown), obtained a federal grantto demonstrate the superiority of comprehensive over fragmented SCIcare. Photo courtesy of Craig Hospital Archives. Alain Rossier(right) ...John Young stated that a “Model System must be ableto meet the needs of a person with SCI by competently treating thedirect injury as well as all organ systems affected (of which thereare many); the functional deficits that result, by providingtraining and equipment; the psychological adjustments that must bemade; the vocational/avocational pursuits that must be changed; andthe providing of long-term specialized care.” He also outlined thenecessary components of such a system, which must include emergencymedical services; emergency trauma care (at a trauma center); acutehospital care; acute rehabilitation care; and ongoingrehabilitation treatment (47,48).
Finally, Alain Rossier (1930–2006) (Figure 12), born inSwitzerland, was strongly influenced by Guttmann and was alsoinfluential in establishing SCI units in his country. He also spent11 years working in the United States at the West Roxbury VAHospital, MA (49). He proved to be a powerful advocatefor veterans with SCI and convinced the VA that more VA hospitalsshould have SCI units and that these units should be equipped tomeet all their patients' medical and social needs throughout theirlives.
Consequently, to this day, patients with SCIrequiring readmission to the designated VA hospitals are admittedto the SCI unit regardless of whether their status is acute orchronic (unless they require intensive care). Today, this stands incontrast to most health care payers, who authorize payments to SCIcenters for acute rehabilitation or for rehabilitation related tochronic issues that can be resolved with a short-term admission.More and more non-VA patients with acute medical problems, eg,acute UTI, are admitted to acute general hospitals, while patientswith chronic medical problems, eg, decubitus ulcers, are admittedto long-term care facilities or are treated at home. This systemexposes the patient to fragmentation of care and to the risk ofcomplications, as the staffs in these settings are less acquaintedwith the special needs of patients with SCI. In settings wherethese conditions prevail, it is important that therehabilitationist bring the principles developed by these heroesand others to the patient. The present challenge is, how?
Go to:IN THE PRESENT—AN AILMENT TO BE TREATED
If one were to ask where the work of these heroes aswell as that of many others (eg, Key of South Africa, Botterell ofCanada, Holdsworth of the UK, Meineke of Germany, Dolfus of France,Chahal of India, Nakamura of Japan, Sarias of Spain, and Stover ofthe US, to mention a few) have brought us today, we could point tothe advances made in medical care; longevity; rehabilitationservices, including mobility and self-care; environmentaladaptations and legislation; and the numerous organizations pledgedto mainstream the lives of persons with SCI and advance the searchfor a cure. A brief sampling of these is mentioned here.
Medical Care
The Spine
As noted, instruments and techniques now exist toassure spinal stability, obtain reductions, maintain alignment, andthereby avoid the pain and further disability caused by a deformedspine (9). In addition, imaging capabilitieshave expanded significantly, not only with respect to the abilityto correlate MRI with impairment (50,51) and prognosis (52,53), but with new MRI applications suchas magnetic resonance imaging–diffusion weighted imaging(54,55), which allows imaging of the tractswithin the spinal cord; functional MRI (56,57); and MRI spectroscopy(58,59).
The Neurogenic Bladder
Advances in this area are the reason whypyelonephritis is no longer the “end condition of the paraplegic.”These include antibiotics to treat and prevent infection of thegenitourinary (GU) tract; anticholinergic medications to maintaincontinence and bladder compliance; less invasive ways to removebladder and kidney stones, eg, electrohydraulic lithotripsy (EHL)and extracorporeal shock wave lithotripsy (ESWL); urodynamics tohelp us unravel the mystery of the neurogenic bladder and recommendthe best treatment approaches; and surgical procedures to enhancebladder storage capacity, facilitate bladder emptying, or increasethe ease of catheterization. These and other treatments haveenhanced social continence and quality of life and have preventedmany of the complications that previously shortened life(60–65).
Sexuality
Men with SCI have benefited from the development oforal agents to treat erectile dysfunction, eg, sildenafil citrate,as well as the injectable prostaglandin E1 (alprostadil) for thosewho do not respond to oral therapy. Since many men with SCI alsohave ejaculatory dysfunction, their ability to father a child bymeans of vibratory or rectal electric probe ejaculation, combinedwith in-vitro fertilization, has been greatly enhanced so thatfatherhood is now commonplace. Women with SCI have also benefited,particularly from safer labor and delivery and if necessary, safercesarean sections due to advances in surgery mentioned earlier.Both men and women have the opportunity for more satisfying sexualrelations (65–70).
Pain
Neuropathic pain has long been a problem for manypersons with SCI (50). The discovery that certainanticonvulsant and antidepressant medications can suppress orrelieve pain perceived by the patient either at the level of injuryor diffusely below it has improved the quality of life for many.Invasive procedures such as implantable spinal cord stimulators andthe infusion of morphine and clonidine intrathecally have provedhelpful in selected cases (71–76).
Spasticity
Involuntary movement and involuntary resistance topassive movement occur typically in persons with SCI above theconus level. These movements can become very strong and haveimpeded many from achieving independence in activities of dailyliving. Oral agents such as baclofen, tizanidine, and dantrolenehave been helpful in reducing spasticity (77). However, the arrival of intrathecalbaclofen, which is used to treat those who do not respondsufficiently to oral medication, has proved to be a breakthrough(78,79). Botulinum toxin, when injected intoa few offending muscles, has also been very helpful(80,81).
Advances in many other areas important to individualswith SCI, including the skin, bowel, bone, lung, and cardiovascularsystem, have also been made but are too numerous to mention here.Suffice it to say, people can be kept healthy and more comfortablebecause of them. All this has fostered their re-entry intosociety.
Longevity
In years past, as noted above, the leading cause ofdeath among persons with SCI was renal failure. Today, however,significant advances in urologic management have resulted indramatic shifts in the leading causes of death. Persons enrolled inthe National SCI Statistical Center Database since its inception in1973 have now been followed for more than 30 years after injury.During that time, the causes of death that appear to have thegreatest impact on reduced life expectancy for this population havechanged and are now pneumonia, pulmonary emboli, and septicemia(84,85). More importantly, people with SCIare living longer (84).
Rehabilitation Services
In addition to the expert clinical, hands-ontreatment now available to individuals with SCI both during acuterehabilitation and during ongoing outpatient care, especially inspinal centers, they can benefit from advances in technology thathave yielded better equipment.
Power wheelchairs can now perform weight-shiftingfunctions by tilting and/or reclining. They can be controlled bymechanisms other than the joystick, eg, head control, sip and puff,and voice and eye movement. This has helped individuals with hightetraplegia expand their mobility with less stress on the shoulderjoints (86,87).
Manual wheelchairs are now lighter, making themeasier to propel and load into a vehicle. They can also be equippedwith power-assist wheels, allowing people with less upper bodystrength to push farther (88).
Lightweight orthotic devices for both upper and lowerextremities have made donning and doffing easier and decreasedenergy cost for ambulatory persons (89,90).
Computer interfaces have allowed individuals withhigh tetraplegia to access the Internet and use other computerapplications, permitting them to experience the benefits (and thecaveats) just like anyone else (91,92).
Pressure mapping to help select the best wheelchaircushion has proven useful to all wheelchair users but especially toindividuals more vulnerable to pressure ulcers, ie, those whocannot perform a manual weight shift or who have severe glutealmuscular atrophy or scars on the weight-bearing surface(93,94).
Body weight–supported treadmill ambulation has bothresearch and clinical applications. Although research is stillongoing on this equipment, it is now proving clinically useful as atraining device for persons with marginal ambulatory capability. Ithas thus far been found useful as an adjunct to the treatment ofpatients with some preserved motor function (ASIA Impairment ScalesC and D) (95).

Other technological advances have improved theself-care, mobility, and independence of persons with SCI; theyinclude functional electrical stimulation (89), speaking valves for tracheostomies,and environmental control systems (96).
Environmental Adaptations/Legislation
Environmental Control Systems
What is sophisticated and extremely useful for thosewho can afford it is the ability to control devices within the homefrom a remote source, eg, wheelchair or bedroom. This might includethe climate control panel, radio/TV/CD player, alarm systems, doorlocks, and other vital functions within the person's home(96).
Home Modifications
Centers providing comprehensive rehabilitation haveplanned their discharges from acute rehabilitation at the pointwhen the patient's abilities matched his/her home environment.Usually, the environment has to be modified to effect this match.This often includes the installation of ramps; widening ofdoorways; altering the bathroom, kitchen, and bedroom; and soforth. There is usually nothing sophisticated about theimplementation of these changes. The challenge is often gettinginsurers to pay for them.
Legislation
The Americans with Disabilities Act signed byPresident George H. W. Bush in 1990 was a landmark piece oflegislation that declared that Americans with disabilities haveequal rights to the environment, employment (if otherwisequalified), public transportation, accommodations, services, andeducation. By all accounts, it was a major breakthrough for personswith SCI, as well as those with other disabilities(97).
Organizations
Many consumer groups have formed throughout thenation and the world to promote the interests of individuals withSCI. They run the gamut in their mission statements. Some areprimarily social, some political, some educational, somephilanthropic, eg, funding research, while others have combinationsof these purposes. One cannot list all of them here but 3 certainlystand out because of their size: The National Spinal Cord InjuryAssociation, Paralyzed Veterans of America, and United SpinalAssociation.
Similarly, many professional groups have formed,usually declaring educational and/or scientific goals for theirorganizations. The International Spinal Cord Society (ISCoS)changes its venues yearly, routinely combining its annualscientific meeting with that of the national SCI organization ofthe host country. In the US, the American Spinal Injury Association(ASIA) and the American Paraplegia Society (APS) each have annualmeetings. ASIA and ISCoS have jointly produced the InternationalStandards for Neurological Classification of SCI. This has nowbecome the gold standard clinical measurement tool used for outcomemeasurement in SCI research on humans (98).
Further, many organizations have formed with at leastone of their objectives being the finding of a way to cure orreverse the damage caused by injury or other pathologic processesto the spinal cord. One of them, the International Campaign forCures of Spinal Cord Injury Paralysis (ICCP) has at present 9member organizations: The Christopher Reeve Paralysis Foundation,The Miami Project to Cure Paralysis, The Paralyzed Veterans ofAmerica, the French Institute for Spinal Cord Research, The JapanSpinal Cord Foundation, The Rick Hansen Man in Motion Foundation,Spinal Cure Australia, Spinal Treatment Australia, and TheInternational Spinal Research Trust. By their names, it is clearthat “cure” is their raison d'etre. Other organizations at theforefront in this effort are the International Collaboration onRepair Discoveries (ICORD), the North American Clinical TrialsNetwork (NACTN), and the European Clinical Trials Network (EUCTN).In addition, there are many smaller groups, often university based,such as “Mission Connect,” which is funded through the efforts ofthe Institute for Rehabilitation and Research (TIRR) in Houston,Texas.
Governmental organizations have also played no smallrole in supporting research activities. These include the WorldHealth Organization (WHO), the National Institute for Disabilityand Rehabilitation Research (NIDRR), the National Institutes ofHealth, especially the National Center for Medical Rehabilitationand Research (NCMRR), and the National Institute for NeurologicalDiseases and Stroke (NINDS). Likewise, as we shall see, thepharmaceutical industry is conducting research investigationsincluding clinical trials.
All the resources of these groups are working towardbringing us to the day when we can declare a cure for SCI.
Go to:IN THE FUTURE—AN AILMENT TO BE CURED
The following organizations are planning for thesound implementation of clinical trials as interventions uncoveredby basic science researchers come on line. The ICCP has taken theinitiative by producing 4 reports thus far (99). At the first meeting, topicsdiscussed included the prevalence and incidence of SCI, bothtetraplegia and paraplegia, in countries where they are known; thenatural history of recovery of neurologic function from informationcontained in the NSCISC Database and other sources; and thestatistical power required to conduct clinical trials. At thesecond meeting, outcome measures appropriate to studies of acute,subacute, and chronic SCI were discussed, along with the importantdifferences between parameters that measure axonal connectivity andthose that measure function. It is important not to confuse orcommingle the two. At the third meeting, inclusions and exclusioncriteria were addressed, along with the ethics of how they affectcontrol groups. Finally, the fourth meeting reviewed the overallprinciples involving clinical trials and how they pertain to SCI,emphasizing randomized prospective clinical trials (RPCT),multicenter trials (due to the relatively low incidence of SCI),the importance of blinding, and the importance of the adherence tothe ethical principles of the Declaration of Helsinki(100) and the Belmont Report(101). This effort has laid thegroundwork for multicenter and multinational collaboration in theconduct of clinical trials within the ambit of NACTN and EUCTN(102).
Clinical trials are in fact underway; many utilizingnew discoveries developed by the pharmaceutical industry in Europe,North America, and Asia (103). These include: (a) theProneuron Phase II trial using autologous incubated macrophages foracute SCI (104); (b) the BioAxone Cethrin trialusing the Rho antagonist BA-210 (Cethrin) for acute SCI(105); (c) the University of Calgarytrial, using minocycline (an antibiotic with cytokine, freeradical, and matrix metalloproteinase inhibition properties) foracute SCI (106); (d) the Aventis HP-184 trialemploying this substance in chronic SCI in which some motorfunction has been preserved—this substance is similar to 4-aminopyridine (4-AP); (e) the Novartis trial using the anti-NoGoantibody, which reverses the inhibiting effect of NoGo onoligodendrocytes for acute SCI (107); (f) the Geron Corporation trialusing implanted oligodendrocyte precursor cells for chronic SCI(108,109); (g) transplantation of fetal andautologous olfactory cells into the spinal cord for chronic SCI intrials in Portugal and China (110,111).
Clinical trials already completed include thosestudying the effects of methyl-prednisolone (10,112–114), GM-1 ganglioside(11,115), 4-AP (116–118), and body weight–supportedtreadmill ambulation (95). Thus far, in sum, these studieshave proved inconclusive.
Research scientists at the animal laboratory levelhave developed multiple strategies for studying and repairing theinjured spinal cord including both acute and chronic subjects(Table1). These efforts have been quietly taking place formore than a decade and have evolved into numerous investigationsapproaching the problem from different angles. These strategiesinclude:
Table 1The Future: Animal Laboratory InvestigationStrategiesA. Reduce the Effects of the Damage
This can be accomplished or aided by maintainingcirculation and oxygenation and creating a favorable milieu(realign and stabilize) (9). Partially damaged neural tissue mayalso be protected by the reduction of neurotoxins and freeradicals, eg, by methylprednisolone or glutamate-receptor (eg, AMPAand NMDA) antagonists (119,120); the reduction of inflammation, eg,by cytokine, Rho, tumor necrosis factor, and interleukin 10blockers; and by the reduction of apoptosis, eg, by calpains ornitric oxide inhibitors (104,121–125).
B. Encourage Correct Neuron Function/Connections Via a NerveBridge
This can be done in 3 ways: 1. With Cells:Schwann cells (126–128); olfactory ensheathing glialcells (125,126,128,129); astrocytes (131); re-engineered fibroblasts orother cell types (132,133). 2. With Matrix Modifiers:These include netrins (134) and neural glues, eg, PEG/synthetichydrogels (135–137). 3. With Nerve Grafts:ie, peripheral nerve implants into the spinal cord after removal ofglial remnants (137).
C. Enhance Regeneration/Axon Growth
Several interesting approaches have shown promise inanimal studies. These include inhibitor-neutralizing antibody(anti-NoGo) (138); neurotrophin 3 (139); acidic fibroblast growth factor(AFGF) (139); brain-derived neurotrophic factor(BDNF) (140); and Rho antagonists(105).
D. Replace Lost Nerve Cells
Currently, fetal tissue implants (141, 142) and stem cells (143) are being studied.
E. Inhibit Scar/Gliosis Formation
Both decorin (144) and chondroitinases(126,145) have shown promise in work donethus far.
F. Reduce Neurocircuit Deficits
Both potassium-channel blockers (118,121) and sodium-channel blockers(121) are being studied for this purpose,along with glutamate-receptor blockers (119).
Go to:CONCLUSION
It is both amazing and gratifying to see the enormousamount of work now being done to solve the mystery of spinal cordregeneration. Most investigators feel the solution to the enigmawill come from this multipronged approach, since very likely genes,molecules, and milieu all play some role (146). With perseverance by thescientists and support from the consumers, like that given by thelate and heroic Christopher Reeve, someday, in the great beyond,even though he lived 5,000 years afterwards, the latter might justconfront Imhotep and say, “See, it can be treated and cured afterall.”
 爱华网
爱华网