[关键词] 转移性结直肠癌;K-Ras基因;基因状态;靶向治疗
[中图分类号] R735.3 [文献标识码] A [文章编号] 1673-7210(2017)03(b)-0041-04
The research progress of the correlation between K-Ras gene and prognosis of metastatic colorectal cancer
CAI Jianfeng GE Wei ZHANG Wenjun ZHENG Yongfa
Department of OncologyⅡ, Renmin Hospital of Wuhan University, Hubei Province, Wuhan 430060, China
[Abstract] At present, colorectal cancer, a serious threat to human health, is a common digestive system malignant tumor. Metastatic colorectal cancer has an important prognosis factor, but the transfer mechanism is not fully clear. Studies have shown that many cancer genes are involved in the transfer process. The Ras gene belongs to the proto-oncogene, when it is activated, it can be transformed into cancer gene and participate in tumor occurrence and development. By detecting the Ras genes in the clinical and according to the state of gene, the targeted therapy can be taken. However, the overall survival of metastatic colorectal cancer has a certain correlation with the status of Ras gene. This review aims to state the research progress of the correlation between K-Ras gene and prognosis of metastatic colorectal cancer.
[Key words] Metastatic colorectal cancer; K-Ras gene; Gene status; Targeted therapy
结直肠癌是目前威胁人类健康的一�N常见恶性肿瘤,其发病率及死亡率在不断上升,其全球发病率在男女恶性肿瘤中分别位居第三、第二位[1-2]。随着对肿瘤抑癌基因及癌基因的深入研究,肿瘤从本质上讲是基因病,肿瘤的发生是多基因、多步骤突变的结果,而原癌基因被激活后具有转化成癌基因导致肿瘤发生的能力。研究显示[3-6],1982年发现在人膀胱癌细胞中有活化的H-Ras基因,此引起了人们对Ras基因的关注。Malumbres等[7]研究发现Ras是一种原癌基因,且Ras基因扩增存在很多肿瘤中,例如胰腺癌、结直肠癌等[8]。Ras基因与人类肿瘤相关的基因有H-Ras、K-Ras和N-Ras三种,分别位于11、12和1号染色体上。然而K-Ras与肿瘤的发生更为密切,K-Ras基因在Ras基因中最易突变[9]。在胰腺癌和结直肠癌中突变率分别为60%~90%、30%~50%,非小细胞肺癌检测到的突变率约为25%[10-15]。对于结直肠癌转移是影响其预后一重要因素,Ras基因突变与患者转移灶切除后的较短总体生存期相关。
1 Ras基因与肿瘤的关系
Ras基因当其被激活后转变为有致癌活性的癌基因,致使表达产物Ras蛋白发生构型的变化继而功能发生变化。Weinstein等[16-17]指出细胞的存活依赖于Ras基因的激活,抑制Ras基因激活会导致肿瘤细胞死亡。Ras基因的激活有方式包括基因点突变、插入与转位以及大量表达,在不同的肿瘤中存在不同的Ras突变。其中K-Ras在Ras基因中最易发生突变对人类癌症影响最大,其具有分子开关的作用在很多信号通路中起重要作用。K-Ras蛋白在信号转到中起重要作用[18-19]与肿瘤细胞的生存、增殖、扩散、迁移及血管生成均有关系。
K-Ras基因分为野生型(处于正常状态)和突变型(处于异常状态)。在结直肠癌中,K-Ras基因外显子2突变的频率是35%~40%[20-21]。K-Ras基因突变发生在肿瘤发生的早期,且原发灶与转移灶的K-Ras基因高度一致。通常认为,K-Ras基因状态不会因治疗而发生变化。被激活的K-Ras基因可使其快速转录翻译,蛋白含量增加,导致细胞克隆性增生形成肿瘤。
2 K-Ras基因与结直肠癌生物学行为 结直肠癌病因至今尚未明确,可能与遗传、饮食因素等相关[22],且结直肠早期易发生远处转移,发生远处转移存活率仅约12%[23],其转移机制尚未完全明确,不同地区转移性结直肠癌临床特点及分子机制也可能截然不同[24]。报道显示[25]:结直肠癌发生腹腔转移后,即使行化疗其预后仍很差,且已成为结直肠癌患者死亡的第二大原因。另有研究[26]对约80%的局部结直肠癌患者实行手术治疗后,约50%的患者因术前存在微转移灶出现复发。目前化疗可用于区域转移的结直肠癌而疗效有一定局限性,对于发生远处转移的结直肠癌疗效更差[27]。因此寻找新的治疗方法是非常必要。临床研究显示[28],K-Ras基因的突变与结直肠癌的发病率有关,且K-Ras的突变情况与肿瘤的预后相关,其在肿瘤的发生、发展、转移等阶段扮演重要的作用[29]。人类癌细胞Ras基因分析显示它们不同与正常细胞的单核苷酸染色体,热点突变的染色体1和2与肿瘤的细胞的转移活性相关[30-31]。K-Ras基因被激活后转变成具有致癌活性的癌基因,影响细胞的生物学行为致使细胞增殖失控癌变。K-Ras基因是表皮生长因子受体(Epithelial Growth Factor Receptor,EGFR)信号通路的一下游基因,EGFR是具有酪氨酸酶活性的一重要的跨膜受体,其中Ras/Raf/ MEK/ERK-MAPK 通路是EGFR下游的一信号通路,当EGFR被配体激活后可启动细胞内的信号转导,通过K- Ras依赖的丝裂原活化蛋白激酶(mitogen-activated protein kinase,MAPK)信号转导通路,影响细胞增殖、分化、凋亡、迁移、黏附、肿瘤血管生成[32]。EGFR信号通路被激活后,K-Ras蛋白先短暂激活,其随后迅速失活,K-Ras激活/失活效应是受控的。而K-Ras基因突变时,可以导致EGFR信号通路持续激活,加速肿瘤细胞增殖,预示肿瘤预后不良。
K-Ras基因突变型,通过影响细胞的生物学行为刺激促进恶性肿瘤细胞的生长扩散,且不受上游EGFR的信号调控影响,对抗EGFR治疗效果差[33]。遂临床上根据K-Ras基因状态的检�y结果决定是否采用EGFR的酪氨酸激酶抑制剂(tyrosine kinase inhibitor,TKI)进行转移性结直肠癌的靶向性治疗。
3 针对转移性结直肠K-Ras基因的靶向治疗
K-Ras基因突变可以导致EGFR-TKI原发性耐药,是预后不良的指标。目前临床上通过检测K-Ras基因状态来预测靶向药物抗EGFR抗体的疗效,是转移性结直肠癌患者进行靶向治疗方案选择的重要指标之一。针对K-Ras野生型的转移性结直肠患者使用抗EGFR抗体治疗[34]。目前获批的抗EGFR单抗有Cetuximab(爱必妥,西妥昔单克隆抗体)、Panitumumab(帕尼单克隆抗体)以及Nimotuzomab(尼妥珠单克隆抗体,泰欣生),前两种药物用于转移性结直肠癌治疗,Nimotuzomab具有与EGFR结合的高亲和力特点,现主要与放疗联合用于治疗EGFR阳性的晚期鼻咽癌[35-36]。
3.1 Cetuximab(爱必妥)
Cetuximab是由FDA在2004年2月批准上市,它是抗EGFR人/鼠嵌合单克隆抗体。在临床上Cetuximab与伊立替康联用治疗伊立替康化疗无效、EGFR阳性的转移性结直肠癌。使用此药物治疗可能会出现超敏反应、呼吸系统疾、眼部疾病以及耐药等,然而病因尚未完全明确[37-39]。
3.2 Panitumumab(帕尼单克隆抗体)
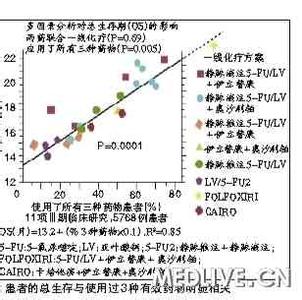
Panitumumab是由FDA(Food and Drug Administration)在2006年9月批准上市的人源化IgG2单克隆抗体。在临床上Panitumumab与伊立替康、奥沙利铂及氟嘧啶联用或者在化疗后用于治疗EGFR阳性的转移性结直肠癌。该药物也有其副作用最常见的是肺纤维化,另可见皮疹、恶心、腹痛等[40]。大样本研究显示:对K-Ras基因外显子2突变的患者通过随机对照试验,采用单独化疗与化疗联合抗EGFR治疗,结果表明患者的PFS(Progression-Free-Survival)及OS(Overall Survival)都未能获益[41]。因此,抗EGFR抗体不推荐用于K-Ras基因外显子2突变的转移性结直肠患者。单纯的化疗不改变Ras基因的突变状态,但当化疗联合Cetuximab或Panitumumab治疗,可能会导致Ras基因二次突变并产生放大效应,这也可能是抗EGFR抗体的潜在作用[21]。另有根据K-Ras基因预测转移性结直肠治疗联合Cetuximab的荟萃分析的结果显示:纳入分析的2188名转移性结直肠癌患者中,K-Ras基因的突变率为38%(829/2188),突变型患者的总体反应率为14%(119/829),野生型患者的总体反应率为39%(529/1359),野生型与突变型患者两者总体反应率相比具有统计学意义(P 4 小结
转移是影响结直肠癌预后的重要原因,K-Ras基因作为与肿瘤发生发展相关的癌基因,临床通过检测肿瘤的基因状态,进行靶向治疗,此为结直肠癌提供新的治疗策略,特别是转移性结直肠癌。目前仅针对野生型K-Ras靶向治疗有一定疗效,突变型治疗结果较差,肿瘤预后仍不容乐观,故其复杂机制及信号通路仍需进一步研究,以便找到的新的治疗策略,从而使晚期结直肠癌患者获益。Cetuximab已批准用于转移性结直肠癌,能否用于早期结直肠癌现处于临床试验阶段,同时Panitumumab与Cetuximab对比分析研究仍需要继续。另外使用靶向药物治疗产生的不良反应也尚未完全清楚, 需进一步观察及深入研究探讨。 [�⒖嘉南�]
[1] Torre LA,Bray F,Siegel RL,et al.Global cancer statistics,2012[J].CA Cancer J Clin ,2015,65(1):87-108.
[2] EI Zoghbi M,Cummings LC. New era of colorectal cancer screening[J].World J Gastrointest Endosc,2016,8(5):252-258.
[3] Der CJ,Krontiris TG,Cooper GM. Transforming genes of human bladder and lung carcinoma cell lines are homologous to the ras genes of Harvey and Kirsten sarcoma viruses[J]. Proc Natl Acad Sci USA,1982,79(11):3637-3540.
[4] Parada LF,Tabin CJ,Shih C,et al. Human EJ Bladder carcinoma oncogene is homologue of Harvey sarcoma virus ras gene[J].Nature,1982,297(5866):474-478.
[5] Santos E,Tronick SR,Aaronson SA,et al. T24 human bladder carcinoma oncogene is an activated form of the normal human homologue of BALB- and Harvey-MSV transforming genes[J].Nature,1982,298(5867):343-347.
[6] Tabin CJ,Bradley SM,Bargmann CI,et al. Mechanism of activation of a human oncogene[J].Nature,1982,300(5869):143-149.
[7] Malumbres M,Barbacid M. Ras oncogene: the first 30 years[J]. Nature Rev Cancer,2003,3(6):459-465.
[8] Bos JL. The ras gene family and human carcinogenesis[J].Mutat Res,1988,195(3):255-271.
[9] Prior IA,Lewis PD,Mattos C. A comprehensive survey ofRas mutations in Cancer[J].Cancer Res,2012,72(10):2457-2467.
[10] Thomas RK,Baker AC,Debiasi RM,et al. High-throughput oncogene mutation profiling in human cancer[J].Nat Genet,2007,39(3):347-351.
[11] Chin L,Tam A,Pomerantz J,et al. Essential role for oncogenic Ras in tumour maintenance[J].Nature,1999,400(6743):468-472.
[12] Macaluso M,Russo G,Cinti C,et al. Rasfamily genes: an interesting link between cell cycle and cancer[J].J CellPhysiol,2002,192(2):125-130.
[13] Knijn N,Mekenkamp LJ,Klomp M,et al. KRAS mutation analysis:a comparison between primary tumours and matched liver metastases in305 colorectal cancer patients[J].Br J Cancer,2011,104(6):1020-1026.
[14] Zorde Khvalevsky E,Gabai R,Rachmut IH,et al. Mutant KRAS is adruggable target for pancreatic cancer[J].Proc Natl Acad Sci USA,2013,110(51):20723-20728.
[15] Campos-Parra AD,Zuloaga C,Manríquez ME,et al. KRAS mutation as the biomarker of response to chemotherapy and EGFR-TKIs in patients with advanced non-small cell lung cancer:clues for its potential use in second-line therapy decision making[J].Am J Clin Oncol,2015,38(1):33-40.
[16] Weinstein IB. Addiction to oncogenes - the Achilles heal of cancer[J].Science,2002,297(5578):63-64. [17] Podsypanina K,Politi K,Beverly LJ,et al. Oncogene cooperation in tumor maintenance and tumor recurrence in mouse mammarytumors induced by Myc and mutant Kras[J].Proc Natl Acad Sci USA,2008,105(13):5242-5247.
[18] Hunter JC,Gurbani D,Ficarro SB,et al. In situ selectivity profiling and crystal structure of SML-8-73-1,an active site inhibitor of oncogenic K-Ras G12C[J].Proc Natl Acad Sci USA,2014,111(24):8895-8900.
[19] Ostrem JM,Peters U,Sos ML,et al. K-Ras(G12C) inhibitor allosterically control GTP affinity and effector interactions[J].Nature,2013,503(7477):548-551.
[20] Kudo T,Satoh T,Muro K et al. Clinical validation of a novel multiplex kit for all RAS mutations in colorectal cancer: results of RASKET (RAS Key Testing) prospective multicenter study[J].WCGIC,2014,25(2):ii73.
[21] Hiroya Taniguchi,Kentaro Yamazaki,Takayuki Yoshino,et al.Japanese Society of Medical Oncology ClinicalGuidelines: RAS (KRAS/NRAS) mutation testing in colorectal cancer patients[J].Cancer Sci,2015,106(3):324-327.
[22] Bailie L,Loughrey MB,Coleman HG.Lifestyle Risk Factors forSerrated Colorectal Polyps: a Systematic ReviewandMeta-analysis[J].Gastroenterology,2016,5085(16):35028-35034.
[23] Siegel R,Naishadham D,Jemal A. Cancer statistics,2013[J].CA Cancer J Clin,2013,63(1):11-30.
[24] Tejpar S,Stintzing S,Ciardiello F,et al.Prognostic and Predictive Relevance of Primary Tumor Location in Patients With RAS Wild-Type MetastaticColorectal Cancer: Retrospective Analyses of the CRYSTAL and FIRE-3 Trials[J].JAMA Oncol,2016,10(1001):3797.
[25] Sasaki Y,Hamaguchi T,Yamada Y,et al.Value of KRAS,BRAF,and PIK3CA Mutations and SurvivalBenefit from Systemic Chemotherapy in Colorectal Peritoneal Carcinomatosis[J].Asian Pac J Cancer Prev,2016,17(2):539-543.
[26] Tebbutt NC,Cattell E,Midgley R,et al. Systemic treatment of colorectal cancer[J].Eur J Cancer,2002,38(4):1000-1015.
[27] Gallagher DJ,Kemeny N. Metastatic colorectal cancer: from improved survival to potential cure[J].Oncology,2010,78(78):237-248.
[28] Taniguchi H,Yamazaki K,Yoshino T. Japanese Society of MedicalOncology Clinical Guidelines: RAS (KRAS/NRAS) mutation testing in colorectal cancer patients[J].Cancer Sci,2015,106(3):324-327.
[29] Vogelaar F,Van Erning F,Reimers M,et al. The prognostic value of Microsatellite Instability,KRAS,BRAF and PIK3CA mutations in stage II colon cancer patients[J].Mol Med,2015,17(10):1-26.
[30] Bos JL. Ras oncogenes in human cancer:a review[J].Cancer Res,1989,49(17):4682-4689. [31] Tsuchida N,Murugan AK,Grieco M. Kirsten Ras oncogene: Significance of its discovery in human cancer research[J].Oncotarget,2016,17(10):8773.
[32] Navas C,Hernandez-Porras I,Schuhmacher AJ,et al.EGF receptor signaling is essential for k-ras ancogene-driven pancreatic ductal adenocarcinoma[J].Cancer Cell,2012,22(3):318-330.
[33] Chung CH,Seeley EH,Roder H,et al. Detection of tumor epidermal growth factor receptor pathway dependence by serum mass spectrometry incancer patients[J].Cancer?Epidemiol Biomarkers Prev,2010,19(2):358-365.
[34] Dienstmann R,Salazar R,Tabernero J. Overcoming resistance to Anti-EGFR therapy in colorectal cancer [J]. Am Soc Clin Oncol Educ Book,2015:e149-156.
[35] Xu S,Ramos-Suzarte M,Bai X,et al.Treatment outcome of nimotuzumab plus chemotherapy in advanced cancer patients:a single institute experience[J]. Oncotarget,2016,7(22):33391-33407.
[36] Liu ZG,Zhao Y,Tang J,et al. Nimotuzumab combined with concurrent chemoradiotherapy in locally advanced nasopharyngeal carcinoma: a retrospective analysis [J].Oncotarget,2016,7(17):24429-24435.
[37] Gelfo V,Rodia MT,Pucci M,et al.A module of inflammatory cytokines defines resistance of colorectal cancer to EGFR inhibitors[J].Oncotarget,2016,30(10):12354.
[38] Yu P,Fan Y,Qu X,et al.Cbl-b regulates the sensitivity of cetuximab through ubiquitin-proteasome system in human gastric cancer cells[J].J BUON,2016,21(4):867-873.
[39] Jonker DJ,O'Callaghan CJ,Karapetis CS,et al. Cetuximab for the treatment of colorectal cancer[J]. N Engl J Med, 2007,357(11):2040-2048.
[40] Ohhara Y,Fukuda N,Takeuchi S,et al. Role of targeted therapy in metastatic colorectal cancer[J].World J Gastrointest Oncol,2016,8(9):642-655.
[41] Karapetis CS,Khambata-Ford S,Jonker DJ,et al. K-ras mutations and benefit from cetuximab in advanced colorectal cancer[J].N Engl J Med 2008,359(17):1757-1765.
[42] Qiu LX,Mao C,Zhang J,et al. Predictive and prognostic value of KRAS mutations in metastatic colorectal cancer patients treated withcetuximab:a meta-analysis of 22 studies[J]. Eur J Cancer,2010,46(15):2781-2787.
[43] Price T,Kim TW,Li J,et al. Final results and outcomes by prior bevacizumab exposure,skin toxicity,and hypomagnesaemia from ASPECCT: randomized phase 3 noninferiority study of panitumumab versus cetuximab in chemorefractory wild-type KRAS exon 2 metastatic colorectal cancer[J].Eur J Cancer,2016,68(8):51-59.
 爱华网
爱华网